A partnership approach to chronic disease prevention
Type of content: About us


Our mission
To build an effective, efficient, and equitable system for the prevention of chronic disease
Latest news
-
Introducing the Prevention Centre’s Scientific Advisory Committee
Date -
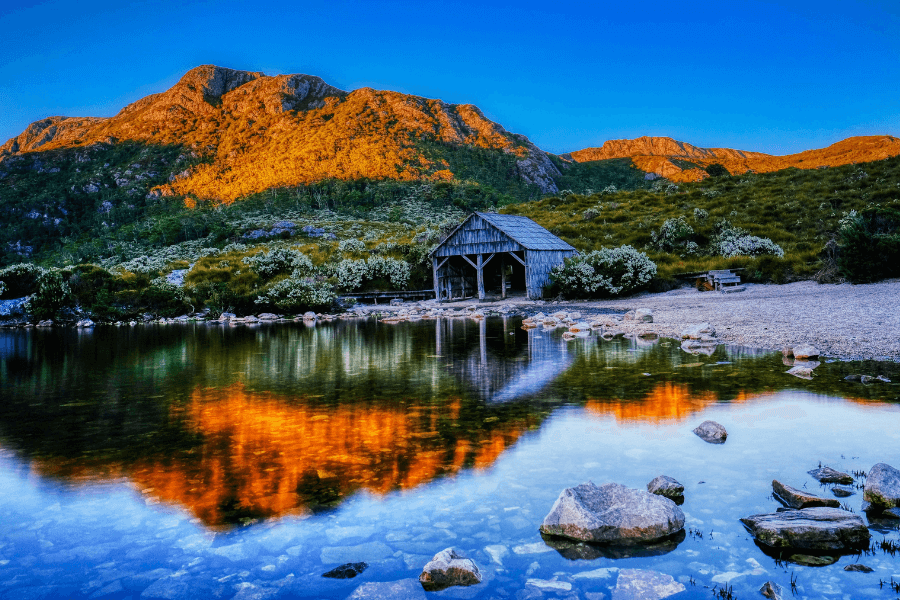
Postcards of prevention: Reflections on community health and wellbeing in Tasmania
Date -
RE-FRESH CRE enters a new generation
Date -
How do we address equity when implementing prevention policy and practice?
Date